The Risks of Cheating
This article originally appeared in our January 2016 newsletter. Due to the [unexpected] overwhelming positive feedback, I decided to improve it and post it here.
I hope you find it helpful.
Stay strong & keep moving forward.
Alan Klapperich
GIG of ECW Branch Manager

While many find it a blessing their condition can be controlled by a "simple diet" change, others consider it a curse of biblical proportions. It's no secret, transitioning to the gluten-free lifestyle can be tough. [Notice the word - lifestyle. The changes required go far beyond just diet.]
A new lifestyle requires the desire to change, knowledge of how to make the change, and the dedication and motivation to stay the course. Yes, it's quite a departure from the previous lifestyle of eating anything from anywhere at anytime.
Barriers to Compliance
When it comes to dietary compliance for the gluten-free diet, there are many barriers that must be broken down:
- Time constraints for cooking or preparing food
- Misinformation
- Lack of knowledge or education (label reading, recognizing gluten)
- Lack of cooking skills
- Ability to manage emotions: depression, anxiety, fear
- Ability to resist temptation
- Feelings of deprivation
- Gluten-Free food availability (may be hard to find)
- Financial restrictions (GF diet can be expensive)
- Social pressures
- Peer pressures
- Travel
- Lack of symptoms
- Effectiveness of the diet (it doesn’t appear to help)
This list seems almost endless, but unfortunately it's still incomplete.
It seems that removing gluten is easier said than done. Give up the foods that you’ve been eating for your entire life? That’s crazy talk!
"I need gluten. I can't live without gluten!"
Ironically, a heroin addict might say something very similar. This is not surprising since narcotics and gluten are addictive. Yes, let’s add "addictive" and "withdrawal symptoms" to the barriers of compliance list.
Addictive? Withdrawal? Seriously?
Yes, yes, and yes. Read on Macduff…

Think of gluten as a string of pearls that must be broken down into individual pearls [known as amino acids].
Humans do not have the enzymes to completely break down gluten into individual amino acids.
Large fragments [known as peptides] of undigested gluten remain after digestion.
Some of those peptides are known as gluteomorphins.
Due to increased intestinal permeability [also known as "Leaky Gut"], the gluteomorphins pass through intestinal wall and enter the blood stream.
Gluteomorphins react with the opiate receptors in the brain, just like heroin and morphine.
This reaction creates a craving - generating the desire for more of the substance.
Julianne Taylor, RN offers up a great explanation on how gluten creates an autoimmune reaction.
http://bit.ly/2vAO4hd or http://bit.ly/3qbRbUp
….and now, back to our regularly scheduled article…
Complications of Untreated Celiac Disease
While it may be easy to rationalize away gluten cheats as simple, temporary aches and pains or as minor [major] inconveniences - beneath the surface, your body could be gearing up for a civil war that would put Gettysburg to shame.

A 2015 study published by The Celiac Center at Beth Israel Deaconess Medical Center (BIDMC) found that 75.5% of the study participants had adequate gluten-free diet adherence.
So what about the other one-fourth (24.5%)? They may be setting themselves up for additional [often serious] medical conditions.
Some of the possible complications of cheating:
- Increased risk of heart attacks & stokes
- Increased risk of blood clots & Deep Vein Venous Thrombosis (DVT)
- Heart muscle damage
- Heart rhythm problems
- Coronary Artery Dissection
- Anemia
- Bone loss
- Cancers
- Ulcerative jejunitis
- Collagenous sprue
- Depression
- Malnutrition
- Neurological disorders
- Infertility
- Miscarriage
- Increased risk of triggering additional associated autoimmune conditions
Complications of Untreated Non-Celiac Gluten Sensitivity
Think you can escape the risks because you have non celiac gluten sensitivity? Sorry, gluten can still rear its ugly head with the likes of:
- Eczema
- Psoriasis
- Depression
- Peripheral Neuropathy
- ADHD
- Multiple Sclerosis
- Ataxia
- Diabetes
- Amyotrophic Lateral Sclerosis (Lou Gerhig's Disease)
- and potentially much more
To learn more about the above list, please check out this link:
by Chris Kresser, M.S., L.Ac
http://bit.ly/1n5wysf
ChChChChanges in Behavior
"Change is not measured in leaps and bounds but in the small steps we take toward a larger goal." ~Claire Dorotik-Nana LMFT
The Barriers to Compliance list above consists of things we can control and things we cannot control. Fear not, this lack of control does not a victim make.
The good news - we get to choose how we react in those situations; if we don't like it - we can change it.
The bad news - change is not always easy and requires effort.
The links below offer some information on how to make the changes that can lead to healthier, happier lives.
GIG of ECW - The Stages of Change: Gluten-Free Edition
by Alan Klapperich
http://bit.ly/GIGECW-Change
"Changes in lifestyle can be some of the biggest modifications we experience particularly if we have a gluten-related disorder. Transitioning to a gluten-free lifestyle turn our lives upside down. So keep calm and let's get prepared. We're going to delve into the gluten-full to gluten-free metamorphosis and give you the knowledge to make it a successful transition. I want to give you a basic understanding of change and the knowledge to make it a successful transition."
NursingTimes.net Vol 107 No 23 06/11/2014 - "Healthier lifestyles: behaviour change"
by Nicola Davies
http://bit.ly/3ozdbYN
"Unhealthy lifestyle choices such as smoking and poor diet are significant and preventable causes of long-term conditions. Nurses are well placed to encourage and support patients to make healthy choices. Through good communication, collaboration and goal-setting, behaviour change is possible. This article discusses evidence for the best ways to initiate and sustain behaviour change."
Note: Updated a link to Nicola Davies’ article. The link originally shared is no longer working
How to Withstand Food Peer Pressure
by Karen Diaz, RD
http://huff.to/1OMFmKx
When you are trying to listen to your body, food peer pressure can be the last straw making you throw in the towel. Here are four important ways to withstand food peer pressure.
Updated:
01/10/21 - Updated links to external resources.
09/30/18 - Added GIG of ECW Stages of Change article.
Celiac Disease: 10 Things Every Gastro Should Know

An excellent article published in August 2015 Clinical Gastroenterology and Hepatology by Amy S. Oxentenko and Joseph A. Murray
Please share this with your healthcare provider!
Text Article: http://www.cghjournal.org/article/S1542-3565(14)01053-2/fulltext
PDF: http://www.cghjournal.org/article/S1542-3565(14)01053-2/pdf
Article Outline
- 1. How to Use Serology to Diagnose Celiac Disease Practical Suggestion
- 2. Can Celiac Disease Be Recognized Endoscopically?
- 3. What Biopsies Should Be Taken to Evaluate for Celiac Disease?
- 4. Which At-Risk Patients Should Be Tested for Celiac Disease?
- 5. How Does One Evaluate for Celiac Disease in a Patient on a Gluten-Free Diet?
- 6. How Is Celiac Disease Managed?
- 7. What Should Be Assessed in the Patient With Newly Diagnosed Celiac Disease?
- 8. How Are Adherence and Response to a Gluten-Free Diet Measured?
- 9. What Is the Approach to the Nonresponsive Celiac Patient?
- 10. What Do We Do With Refractory Celiac Disease?
"Celiac disease (CD) is increasingly common and topical for both the general and medical communities; therefore, gastroenterologists will be called on for expertise in this area. How CD is diagnosed has changed over time, and confusion abounds regarding the use and interpretation of diagnostic tests, which are often confounded by adoption of the gluten-free diet (GFD). Herein, we address 10 important things that gastroenterologists need to know about CD, which are based on current evidence and our experience in Mayo Clinic’s Celiac Disease Clinic."
"There are 10 things that all gastroenterologists should know about celiac disease (CD).
- 1 - The immunoglobulin A tissue transglutaminase is the single best serologic test to use for the detection of CD.
- 2 - CD can be recognized endoscopically, and water immersion enhances villi detection, although a normal endoscopic appearance does not preclude the diagnosis.
- 3 - It is recommended that 4 biopsies be taken from the second part of the duodenum and 2 bulb biopsies be taken at the 9 o’clock and 12 o’clock positions to maximize the sensitivity for histologic confirmation of CD.
- 4 - Consider serologic testing of first-degree relatives, patients with type 1 diabetes mellitus, Down’s, Turner’s, and Williams’ syndromes, as well as those with premature osteoporosis, iron deficiency, abnormal liver biochemistries, and other manifestations of CD.
- 5 - Patients already on a prolonged gluten-free diet (GFD) should be tested for the presence of HLA DQ2 or DQ8, thereby avoiding the need for further evaluation of CD in non-allelic carriers.
- 6 - The basic treatment of CD is a strict, lifelong GFD, enabled by an expert dietitian.
- 7 - Newly diagnosed adults with CD should be assessed for micronutrient deficiencies (iron, B12, folate, zinc, copper), fat soluble vitamin deficiencies (vitamin D), and bone densitometry.
- 8 - All patients diagnosed with CD should have clinical follow-up to ensure response and adherence to a GFD.
- 9 - In those with persistent or relapsing symptoms, the robustness of the original diagnosis should be reviewed, gluten exposure sought, and a systematic evaluation for alternative and associated diseases performed.
- 10 - Evaluate those with refractory disease for malignant transformation."
Celiac Disease Screening Round Up
Updated 08/06/18
Beth Israel Deaconess Medical Center - Celiac Center
University of Chicago - Celiac Disease Center
Celiac Disease Foundation (CDF)
http://bit.ly/2vplMUB
Gluten Intolerance Group of North America (GIG)
Root Cause Medical Clinic
http://bit.ly/2vDSUqE
Mayo Clinic - Mayo Medical Laboratories
Celiac Disease Diagnostic Testing Algorithm (clickable PDF)
https://mayocl.in/2LXTryZ
Celiac Disease Comprehensive Cascade (clickable PDF)
https://mayocl.in/2vqhSut
Celiac Disease Gluten-Free Cascade (clickable PDF)
https://mayocl.in/2OPKaqb
Celiac Disease Routine Treatment Monitoring Algorithm (clickable PDF)
https://mayocl.in/2OMiu5I
Celiac Disease Serology Cascade (clickable PDF)
https://mayocl.in/2M3BqhM
BeyondCeliac.org
http://bit.ly/2OOShDB
Spectrum of gluten-related disorders: consensus on new nomenclature and classification
This is a great handout for your healthcare professional.
Non-Celiac Gluten Sensitivity: The New Frontier of Gluten Related Disorders
Non-Celiac Gluten Sensitivity Where are We Now in 2015?
Carol Rees Parrish, M.S., R.D., Series Editor
08/06/18 - Remove CSA & Dr. Rodney Ford link. Update Beth Israel links. Update Mayo Clinic info. Update NCGS info. Shorten all URLs.
03/02/17 - Added Mayo Labs link
07/02/16 - Added 2013 The New Frontier of Gluten-related Disorders
05/21/16 - Fixed broken links
07/24/15 - Added HealthNow link
Mood, Behavior, Mental Illness and Gluten

The intent here is not to bore you with medical mumbo jumbo [WARNING: medical mumbo jumbo lies ahead], but the takeaway here is simply this:
Gluten has been shown to affect mood, behavior, and cognitive function.
"The gut is not like Las Vegas. What happens in the gut, does not stay in the gut." ~ Dr. Alessio Fasano
Remember, gluten can affect any, and every organ in the human body – the brain and nervous system are not exempt – even without the presence of celiac disease. Science & medicine are discovering more connections as time goes on.
The statistics for mental illness in the United States are staggering.
- One in four [25%] adults experience mental illness in a given year.
- One in 17 [approx 6%] live with serious conditions like: schizophrenia, major depression, bipolar disorder.
- Approx. 1.1% of adults live with schizophrenia.
- Suicide is the tenth leading cause of death in the US (more common than homicide) and third leading cause for ages 15 to 24 year olds.
- More than 90% of those who die by suicide had one or more mental disorders
- In 2010, the Center for Disease Control reported 38,364 suicides per year – about 14% more than motor vehicle crashes.
- $193.2 billion – Lost earnings per year due to mental illness.
- Veterans account for 20% of suicides. 22 per day.
- Mood disorders (like depression) are the third most common cause of hospitalization for youth and adults 18 to 44.
After looking at those statistics, sadly, I suspect just about every family has had some experience with mental health issues in some form, be it directly or indirectly. I am no exception. My father was a diagnosed Paranoid Schizophrenic. Like many, he was not compliant with his medication regimen nor did he seek on-going professional help. The consequences of his choices are still rippling outward today, almost 50 years after his suicide. I will always wonder if removing gluten would've altered our family's history; without question it has altered my future.
Most mainstream medical professionals do not associate gluten with neurological/behavioral disorders. This is unfortunate because Dr. Marios Hadjivassiliou, Professor of Neurology at Sheffield, UK Teaching Hospitals, stated in 2002,“Gluten sensitivity can be primarily and at times exclusively a neurological disease.” http://bit.ly/1qXJdf3
Dr. Hadjivassiliou has done extensive work with a neurological condition called Gluten Ataxia. This condition is characterized by the loss of balance and coordination, visual disturbances, tremors, difficulty in walking. Living Without Feb/March 2011 has an excellent article on this topic - http://bit.ly/1u24c0q
Dr. Hadjivassiliou is not alone in his discoveries. Dr. Rodney Ford, a Pediatric Gastroenterologist/Allergist from Christchurch New Zealand, wrote this medical hypothesis paper in 2009 titled - “The Gluten Syndrome: A Neurological Disease” - http://bit.ly/1tkM58j
“Gluten can cause neurological harm through a combination of cross reacting antibodies, immune complex disease and direct toxicity. These nervous system affects include: dysregulation of the autonomic nervous system, cerebella ataxia, hypotonia, developmental delay, learning disorders, depression, migraine, and headache. If gluten is the putative harmful agent, then there is no requirement to invoke gut damage and nutritional deficiency to explain the myriad of the symptoms experienced by sufferers of celiac disease and gluten-sensitivity. This is called ‘‘The Gluten Syndrome” ~ Dr. Rodney Ford.
Dr. Ford has devoted an entire book on the subject of gluten's effect on our brains. I highly recommend “Gluten Brains” - http://bit.ly/GlutenBrains
“Neurologic and Psychiatric Manifestations of Celiac Disease and Gluten Sensitivity”was published in Psychiatric Quarterly in March 2012 and contains a great summary of a variety of gluten-related conditions. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641836/
Neurologic Complications include:
- Gluten Ataxia
- Epilepsy and Seizure Disorders
- Peripheral Neuropathy
- Inflammatory Myopathies
- Myelopathies
- Headache
- Gluten Encephalopathy (Brain Damage)
- White matter abnormalities
Psychiatric Complications include:
- Anxiety Disorders
- Depression and Mood Disorders
- Attention Deficit-Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorders
- Schizophrenia
The Celiac Disease Foundation created an excellent resource on celiac disease (and non-celiac wheat/gluten sensitivity) and mental health. It's meant to be shared with healthcare providers.
http://ow.ly/en1M30ghVy8
A wide range of psychological problems can arise for those with untreated celiac disease or non-celiac wheat sensitivity. Initially there may be a misdiagnosis of psychiatric illness due to some of the neurological and psychiatric symptoms that can be seen in untreated disease. Once diagnosed, there may be difficulty adjusting to a new diagnosis of chronic illness and adherence to a gluten-free diet."When a Mental Health Referral Is NeededA wide range of psychological problems can arise for patients with untreated celiac disease or non-celiac wheat sensitivity. These can include difficulties adjusting to a new diagnosis of chronic illness as well as dealing with adherence to a gluten-free diet and other aspects of disease management. Protracted duration of emotional or behavioral symptoms, greater severity of symptoms, and/or significant impairment in functioning are indicators of potential need for mental health treatment. These include:
• Finding little or no pleasure in life • Feeling worthless or extremely guilty • Crying a lot for no particular reason • Withdrawing from other people • Experiencing severe anxiety, panic or fear • Having big mood swings • Experiencing a change in eating or sleeping patterns • Having very low energy • Losing interest in hobbies or pleasurable activities • Having too much energy, having trouble concentrating or following through on plans • Feeling easily irritated or angry • Experiencing racing thoughts or agitation • Hearing voices or seeing images that other people do not experience • Believing that others are plotting against you • Wanting to harm yourself or someone elseWhen A Medical Evaluation Is NeededInitially those with celiac disease or non-celiac wheat sensitivity may be misdiagnosed with a psychiatric illness due to some of the neurological and psychiatric symptoms that can be seen in untreated disease including:• Mood changes • Anxiety • Fatigue • Difficulties with concentration and attention • Sleep difficulties • Decrease appetiteCeliac Disease and Gluten-Related Conditions Psychological Health Training ProgramThe Celiac Disease and Gluten-Related Conditions Psychological Health Training Program was created by the Children’s National Health System in partnership with Celiac Disease Foundation, and was made possible by a generous grant from the Resnick Family. This continuing education program provides a tool kit for medical and mental health practitioners to identify and treat patients living with celiac disease and other gluten-related conditions.Watch the Psychological Health Training Program Webinarhttp://bit.ly/2hI3QgTPsychological Health ManualAvailable both as an interactive manual and as a pdf document, the goal of this manual is to increase medical and mental health providers’ awareness of celiac disease and non-celiac wheat sensitivity in pediatric populations. However, it’s lessons apply to adult populations, and is a useful tool for patients and caregivers to better understand the disease.Read the Psychological Health Training Program Manualhttp://bit.ly/2iwf2wV
Depression
Depression is a medical condition that interferes with daily life; affecting thoughts, feelings, behavior, mood and physical health for extended periods of time. Some people may only have one episode of major depression in their lifetime, but often times it is a recurrent issue.
In celiac disease, nutritional deficiencies from intestinal damage may also contribute to depression. Lack of B-vitamins, specifically B-12 and folic acid have been linked.
Reports of depression in those with celiac disease began appearing in the 1980s. In 1982, a Swedish study reported “Our results suggest that depressive psychopathology is a feature of adult coeliac disease and may be a consequence of malabsorption” http://1.usa.gov/W3jKEB
A 1998 study shows about one third of diagnosed celiac patients also suffer from depression. Celiac adolescents have higher than normal rates of depression (31% vs 7% of adolescents without celiac). http://bit.ly/1qUGi2S
A large Swedish study published in 2007 compared almost 14,000 celiac patients against almost 67,000 healthy people. Researchers found that celiacs are 80% more likely to experience depression than the general population. They also looked at the celiac-depression relationship in reverse. They found those with depression had a 230% increased risk factor of having celiac disease. http://1.usa.gov/1pApGlN
Women with celiac disease have higher rates of depression than the general population. The risks were highest in those that were not compliant with the gluten-free diet. Even when compliant, women still had higher risks of depression over those without celiac. http://bit.ly/W3nKoE
According to Dr. Tom O'Bryan, children have a 40% increase risk of suicide. Those children with intestinal inflammation [no villi damage yet] have a 96% increased risk. http://bit.ly/1rJ7wjo
Adults diagnosed with celiac disease and/or intestinal inflammation have increased suicide risks as well. Another large study published in 2011 from Sweden shows those with with celiac disease [intestinal damage] had a 55% increased risk factor. Those with intestinal inflammation [no villi damage] had a 96% increased risk. http://1.usa.gov/Z4DFFk
More Gluten & Depression Studies
“A study has now demonstrated that gluten is independently associated with depression in patients with NCGS.” - http://1.usa.gov/1tZiAqc
“Exposure to gluten specifically induced current feelings of depression.” - http://1.usa.gov/1ucfDBZ
“Lifetime depressive symptoms may be present in one third of the CD patients who adhere to gluten-free diet. Long-term adherence to the gluten-free diet may reduce the risk of current depressive symptoms.” - http://1.usa.gov/1qqWZpe
Schizophrenia
Schizophrenia is a brain disorder that distorts thinking, behavior, emotions, the perception of reality. Delusions [believe people are try to control them or plotting against them] and hallucinations [hearing voices] are common symptoms.
There have been observations of Schizophrenia and gluten dating back to the 50's & 60's – also known then as “Bread Madness”.
In 1953 Dr Lauretta Bender started seeing increased incidences of celiac disease in those with childhood schizophrenia.
In 1961 Harold Graff, M.D. and Allen Handford M.D. published the case study, “Celiac Syndrome in the Case Histories of Five Schizophrenics”, about five patients with a history of schizophrenia and celiac disease who happened to be admitted to the same psychicatric hospital over the course of 365 days. A most curious observation in facility that had few admissions over the course of a typical year. http://bit.ly/1uFm56w
Dr. F. Curtis Dohan spent most of his career drawing connections between wheat and schizophrenia. He too noticed a number of patients with schizophrenia also had celiac disease – potentially 50 to 100 times the rate that would be expected by mere chance. Beyond these connections, he reported that a gluten-free diet improved some of the newly diagnosed schizophrenics, but not all. 2 out of 17 improved. http://bit.ly/1nhCHLw
In 1966 Dohan published “Wheat Consumption and Hospital Admissions for Schizophrenia During World War II”. He analyzed the the decreases in hospital admissions for schizophrenia during the wheat shortages in Finland, Norway, Sweden, Canada and the United States during World War II. http://bit.ly/1q0nRxU
Like many pioneers in their field, Dohan was often ridiculed and marginalized for his work [opioid research in mental illness], but he continued publishing his findings. Dohan also demonstrated that schizophrenia was almost non-existent in South Pacific cultures where little to no grains were consumed. When those cultures began to westernize their diet with the consumption of wheat, barley beer, and rice, the prevalence reached European levels. http://1.usa.gov/1wYpKja
Did Dohan find a “scientific smoking gun” linking gluten and schizophrenia – not exactly according to some experts, but his work is now proving to be quite interesting and now beginning to be validated.
It has only been over the last decade or so that experts have shown gluten's effects on the nervous system. Even to this day experts are still looking indisputable evidence connecting the two conditions.
In 2012, another study revealed that people with schizophrenia are much more likely than the general population to have an immune response to gluten. When those with schizophrenia and a documented immune response to gluten tried a gluten-free diet, they got better. These results are very promising for those suffering from a neuro-degenerative condition where little else works.
Not everyone with schizophrenia will see improvements on a gluten-free diet. New research is indicating about 20% may experience measurable improvements. Dr. Alessio Fasano's team have found that roughly 1 in 5 patients with schizophrenia have elevated levels of tTG6 (a new marker indicating gluten-sensitivity). Those patients put on a gluten-free diet were able to control their condition without medication. Promising results indeed!
More Gluten & Schizophrenia Studies
“Gluten Sensitivity and Schizophrenia” a PowerPoint presentation by Deanna Kelly, Pharm.D, BCPP Professor of Psychiatry at Univ. of Maryland School of Medicine.
http://bit.ly/2f4x8pv
“Emerging scientific literature contains several reports linking gluten sensitivity states with neuropsychiatric manifestations including autism, schizophrenia, and ataxia.” http://1.usa.gov/1tkxTvQ
“A drastic reduction, if not full remission, of schizophrenic symptoms after initiation of gluten withdrawal has been noted in a variety of studies. However, this occurs only in a subset of schizophrenic patients.” - http://bit.ly/2kIpUtQ
“Five biomarkers of gluten sensitivity were found to be significantly elevated in patients with non-affective psychoses (schizophrenia) compared to controls.” - http://1.usa.gov/1vXlWL1
Al Klapperich
Branch Manager
Gluten Intolerance Group of East Central WI
Updated: 11/05/17 - Add Celiac Disease Foundation information.
Updated: 02/12/17 - Fix broken schizophrenia study linkUpdated: 11/05/16 - Updated Deanna Kelly's presentation link.
Updated: 10/09/16 - Add Susan William's letter.
Gluten Contamination Eliminiation Diet
BMC Gastroenterology 2013, 13:40 - http://bit.ly/12vSGuD
Researchers at Johns Hopkins and Center for Celiac Research at Massachusetts General looked at cross contamination of gluten-free products found in a traditional gluten-free diet. They studied 17 patients who had Non Responsive Celiac Disease (NRCD). 6 of these patients met the criteria for Refractory Celiac Disease (RCD).
NRCD is a general classification term for patients with persistent symptoms and/or intestinal damage despite following a gluten-free diet.
RCD is a subset of NRCD. RCD is found in adults; middle-aged to elderly. It's never seen in children. In most cases, failure to improve on a gluten-free diet is not RCD. RCD is also further broken down as RCD1 and RCD2. RCD2 has a higher risk of developing intestinal cancer and 5 year death rate of 50-60%.
Participants of this study were put on a Gluten Contamination Elimination Diet (GCED) for three to six months. This diet consists of whole, unprocessed foods. It was designed to eliminate exposure to any possibility of gluten cross contamination from packaged/processed foods – including those labeled gluten-free. Patients were given sample menus and were asked to keep a food record.
Foods used in the study Allowed Not Allowed Grains - Plain, unflavored, brown and white rice Grains - Millet, sorghum, buckwheat or other inherently gluten-free grains, seeds, or flours Fruits/Vegetables - All fresh fruits & vegetables Fruits/Vegetables - Frozen canned or dried Proteins - Fresh meats, Fresh fish, Eggs, Dried beans, Unseasoned nuts in the shell. Lunch meats, Ham, bacon, Other processed, self-basted or cured meat products Dairy - Butter, yogurt (unflavored), milk (unflavored), aged cheeses Dairy - Seasoned or flavored dairy products, Processed cheeses Condiments - Oils, vinegar, honey, salts Condiments - Flavored and malt vinegar Beverages - 100% fruit/vegetable, Gluten-free supplemental formulas, Gatorade, milk, water
The study revealed some interesting results.
- 14 of the 17 patients experience resolution of their symptoms and normal blood/biopsy results on the GCED.
- 11 of the 14 successfully returned to a traditional gluten-free diet without return of symptoms.
- Of the 3 patients that could not return to traditional gluten-free diet - one had a return of symptoms each of the three times they tried to return.
- 5 of the 6 patients with RCD has full resolution of their symptoms and no longer met the criteria for RCD
The important take away from this study has to do with ferreting out those that truly have Refractory Celiac Disease. Due to the seriousness of RCD, it is important accurately diagnose this condition.
The researchers found it interesting that 79% of the test subject were able to return to their traditional gluten-free diet.
While the researchers commented on the ability to return to a traditional gluten-free diet, they didn't really discuss this aspect. It certainly raises several questions.
1) Once healed, why where most patients able to resume the traditional GF diet?
2) Long-term will they be able to remain on a traditional GF diet without further complications?
3) Could those now successfully following a traditional GF diet benefit from the GCED?
Better living thru Gluten-Free Chemistry

If you think determining the gluten-free status of food is difficult, try doing it with prescription medications! It's difficult at best to determine it by reading the ingredient label, and getting a pharmaceutical company to say if their product is gluten-free is like pulling teeth. Ugh...
The Food Allergen Labeling Consumer Protection Act of 2004 [FALCPA] requires packaged food items to declare wheat and other allergens, but medications do not fall under the umbrella of the FDA's rulings.
Medications contain the active ingredient, but generally it needs to combined with something else - something called an excipient.
What's an excipient?
It's a pharmacological term used for an inert substance that acts as a carrier for the actual drug itself [the "active ingredient"]. Excipients are also used as a filler to bulk up formulations to ensure proper and accurate dosages and as a binder [pill form].
For an extensive list of excipients, see glutenfreedrugs.com Excipients List; complete with descriptions.
Drugs.com has an excellent Inactive Ingredients page. Does not address gluten, but very in-depth explanations of each item.
Starches found in medications can include:
- Corn (most common)
- Cyclodextrins*
- Dextrates*
- Dextrin*
- Dextrimaltose*
- Maltodextrin*
- Modified Starch*
- Pre-gelatinized Modified Starch*
- Pre-gelatinized Starch*
- Sodium Starch Glycolate*
- Starch*
- Tapioca
- Wheat
Since drug companies don't have to disclose source of the starch, there is no easy way to tell if certain ingredients are gluten-free. Calling the manufacturer is the only [and best] option.
Common gluten-free excipients include*:
- Acacia
- Alginic acid
- Alpha tocopheral
- Ascorbic acid
- Benzyl alcohol
- Calcium carbonate
- Carboxymethylcellulose
- Citric acid
- Corn starch
- Croscarmellose sodium
- Dextrose
- Docusate sodium
- Fructose
- Glucose
- Hydrogenated vegetable oil
- Hydroxypropyl cellulose
- Lactose
- Magnesium carbonate
- Magnesium stearate
- Matitol
- Maltose
- Mannitol
- Microcrystalline cellulose
- Polydextrose
- Povidone
- Propylene glycol
- Silicon dioxide
- Simethicone
- Sodium benzoate
- Sodium lauryl sulfate
- Sorbitol
- Stearic acid
- Sucrose
- Vanillin
- Xanthan gum
- Zinc stearate
Cynthia Kupper, RD (Executive Director of the Gluten Intolerance Group) states that patches, inhalants, injectables, and liquids/elixirs are not problematic for those following a gluten-free diet. Source: HealthNow's 2010 Gluten Forum DVD
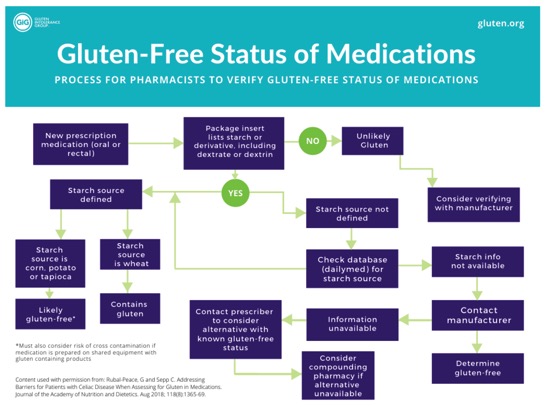
Contained in GIG’s Medications and the Gluten-Free Diet PDF, is a larger version of this pharmacist-created flowchart to aid in the determination of a gluten-free medication.
Here are a few other links of interest:
Bills like this have been submitted since 2013, but they never saw the light of day. Please contact your senators and congressional representatives to let them know this bill is important to you. Find your Senators and Congressional Representatives.
Note: Due to the article's age, any brand name products that are stated as gluten-free, should no longer be considered GF. It's my opinion that any published list of gluten-free products, should not be blindly followed. Since manufacturers can change the ingredient list without notice, the product needs to be verified with each purchase.
Once a pill has been identified, additional information is provided, including brand/generic name, ingredients, and the National Drug File identification number.
Sadly, NFCA no longer offers a free online continuing education program for Pharmacists. However, a PDF is still available: PDF for Pharmacists.
HR 2003: Gluten in Medicine Disclosure Act Update - November 2013:
http://celiac.org/blog/2013/11/06/hr-2003-gluten-in-medicine-disclosure-act-update/
Hopefully you and your Pharmacist find this info helpful.
Al
update 04/29/21 - Add Gluten in Medications Act info.
update 01/12/21 - Update GIG links and graphics. Update links.
update 12/14/19 - Added Gluten and Generic Medications Article
update 04/09/19 - Added CDF Gluten in Medication Disclosure Act of 2019 info.
update 01/12/19 - updated excipient list and note updated GIG’s Medication and the Gluten-Free Diet info
update 09/02/18 - fix broken GIG Medications and Celiac Disease link.
update 01/20/18 - added FDA's Draft guidance document on GF drug labeling.
update 10/19/16 - added AllergicLiving.com's link
update 10/31/15 - Updated GIG's Celiac Disease & Medications link
update 09/12/15 - Added Living Without's - Gluten-Free and More article "Gluten in the Pharmacy"
update 05/13/15 - Added Living Without's - Gluten-Free and More article "Allergens in your Medication"
update 02/23/15 - Added Medscape article "Medications and Supplement Use in Celiac Disease"
update 02/13/15 - Added med research sites and Gluten in Medication Webinar/slides
update 07/29/14 - Added CDF link
update 05/25/14 - Added About.com article.
update 05/25/14 - Added PracticalGastro 2008 & 2009 articles.
update 05/25/14 - Added Delight Gluten-Free Magazine article.
update 03/18/14 - remove link to GREAT Pharmacists training - add link to corresponding PDF
update: 12/14/13 - updated link to GIG's Medications & Celiac Disease educational bulletin
update: 11/9/13 - added Gluten In Medicine Disclosure Act info
update: 9/11/13 - added Living Without's Steven Plogsted interview
update: 05/03/13 - added more info on excipients.
CD more common than 50 years ago
This study looked at blood samples that were collected at Warren Air Force Base between 1948 and 1954. The researchers tested the samples for celiac disease and compared the results from those individuals collected recently. They found young people today are more than 4 times as likely to have celiac disease than the same age group in the 1950's.
Also noted in the study was that patients who did not know they had celiac disease were almost 4 times as likely to have died during the 45 years of follow up.
It's not known exactly why it much more common.
Watch a video of Dr. Murray discuss this study
More details on the study can be found here.
Al's Commentary:
I wonder how much of the increase has to do with the amount of processed foods that exist in the Standard American Diet?