The Tale of Two Nightclubs
Understanding Celiac Disease Through
Motorcycles and Nightclubs
Several years ago, I encountered a recently-diagnosed guy who was having a rough time. His friends would hassle him about his diet, and he was struggling to explain celiac disease to them. As I got to know him, he revealed he rode motorcycles and hung with his buddies in bars. Back then, I came up with this basic analogy to help them understand. I decided to beef it up a bit. While I geared it toward his interests, I think it's generic enough to be understood by everyone.
Indeed, getting family and friends to understand this condition can be trying at times. It doesn't make sense how we can eat something all of our life - then BANG - we can't. Nor do they comprehend how diligent we must be in our diet or the seriousness of gluten infractions. It's our responsibility to educate them the best we can or as much as they will allow us. Be aware; they may not want to hear any of it.
What is Celiac disease?
The Gluten Intolerance Group defines it this way:
"Celiac disease is a chronic, autoimmune disease which is the result of an immune system response to the ingestion of gluten (a protein found in wheat, rye, and barley) in susceptible individuals. This response to gluten damages the small intestine, leading to malabsorption of nutrients and related health issues."
Who can get celiac disease?
"Genetics loads the gun - the environment pulls the trigger. " ~ Dr. Judith Stern, Professor of Nutrition and Internal Medicine University of California at Davis.
How do I get celiac disease?
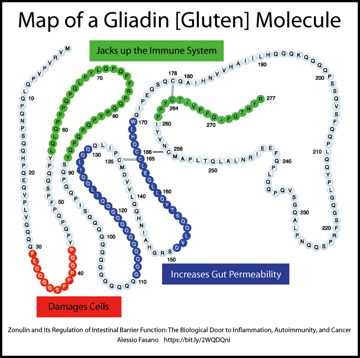
Often we experience an event that is a suspected trigger like surgery, an infection, illness, pregnancy, or possibly extreme stress. Experts don't completely understand the exact reason a person loses their life-long ability to tolerate gluten, but they're working on it. They know that genetics and environment are necessary, but not sufficient to determine if someone will get celiac disease. Three other elements are vital in this equation: a gut that leaks - allowing the gluten to interact with our immune system; an overly-belligerent immune system; and an altered microbial ecosystem in our gut that is known as our microbiome. Of course, one must be consuming gluten in the first place. In today's society, that's almost a given.
What is gluten?
Gluten is the generic term for the proteins found in grains. Wheat [durum, graham, kamut, semolina, spelt, emmer, einkorn), barley [malt], rye [triticale - a hybrid of wheat and rye], and most oats due to cross-contact with gluten are problematic for those with a gluten-related disorder.
I have not heard about celiac disease before, is it new?
Gluten-related disorders such as Celiac Disease, Dermatitis Herpetiformis [an itchy skin manifestation of celiac disease], Gluten Ataxia [unsteady/wobbly walk due to neurologic damage], Wheat Allergy, Gluten/Wheat Sensitivity are not new. Since the introduction of grains during the dawn of agriculture over 10,000 years ago, human-kind experienced problems. During the second century, Aretaeus of Cappadocia, a Greek physician practicing in Rome, observed and documented this condition. In one of his few surviving written works, "The Coeliac Affection," he describes the disease:

"If the stomach be irretentive of food and if it pass through undigested and crude, and nothing ascends into the body, we call such person koiliakos."
If you hadn't guessed, the word celiac [coeliac is the British spelling] comes from the Greek word Koiliakos which means "suffering in the bowels."
The skeletal remains of a young Roman woman buried in a 2,000-year-old tomb in Tuscany showed signs of malnutrition and osteoporosis. DNA analysis revealed she carried two copies of the celiac genes - elevating her risk factor even higher. Experts suspect this woman had untreated celiac disease. What about her diet? Carbon and nitrogen isotope analysis of the bones cannot give us specific details. Still, they suggest she would have consumed more meat, possibly freshwater fish, but limited plants [like wheat].

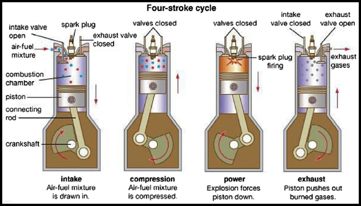
For our body to utilize the food we eat, our digestive system breaks it down into smaller pieces called amino acids. Think of gluten proteins like the drive chain on a motorcycle. Just as the chain consists of individual links, strands of gluten are comprised of amino acids. To break down the strands into digestible amino acids, we need specific enzymes. Those enzymes are like a chain breaker tool. To fully use that chain, we must break it down into individual links.

Engines have gaskets; their purpose is to prevent leakage of oil and water. When gaskets leak, the engine is in trouble. Our gut also has a special gasket; it's called the intestinal epithelial barrier. Unlike gaskets used in engines, our one-cell thick gut gasket is designed to open and close. It opens to allow "friendly" things to pass through like those amino acids. Yet, it also needs to keep out larger items like bacteria, viruses, and fragments of undigested gluten peptides.
Another unusual property of gluten when consumed; it tells our gut gasket to open by stimulating the release of a protein called zonulin. This opening happens in everyone but stays open longer in those with celiac genes due to excess zonulin production. This condition is called increased intestinal permeability, also known as leaky gut. Gluten is not the only thing that can create damage or cause a leaky gut. Just like an engine, when our gut gasket leaks too much, we're in trouble. Gluten sneaks past our epithelial barrier - that’s when the problems start.
What happens when we ingest gluten?
We're going to shift gears (pun intended). Let's compare night clubs or bars and our bodies; today's bar crawl will feature Club 99 and The Crypt. Inside, Club 99's atmosphere is vibrant and inviting. Lots of lush, colorful plants of varied species decorate the room. Tables are neatly aligned and inhabited with diverse and cheerful guests. A beautiful antique bar provides a stunning focal point. Jazz Fusion music plays lightly in the background. Oooo, is that Jean Luc Ponty, I hear? The exterior of the property is well-maintained too. Greeting us at the main door is a chiseled gentleman with broad shoulders, narrow waist, and well-defined biceps bulging out of his stylish Polo shirt emblazoned with a C99 logo. Their security team lurks unobtrusively and quietly in the shadows - waiting and watching. Yes, everything looks quite healthy.


Club 99 illustrates a healthy body inside and out. Our structure is good; we have healthy skin, our intestinal flora and fauna are balanced; everyone works and plays well with others. C99's attentive and well-behaved doorman acts like a "gut gasket" should. He lets good things in and keeps bad things out. C99's security staff is well-trained and evenly tempered - like a healthy immune system. For 99% of the population, their Ninja-like immune system quickly and quietly deals with gluten without incident.
I think you’ll agree, The Crypt is not a good place. Years of damage takes its toll internally and externally. Far too many unsavory characters have taken up residence there, forcing out those who would bring something beneficial to the party. Intensifying an already hostile environment, The Crypt's off duty doorman allows troublemakers inside the club. Conditions are ripe for an epic all-out barroom brawl. “Saturday night's alright for fighting. Get a little action in.” Everything is laid to waste when the overly aggressive security team tears up the place when dealing with the agitators. Shots are fired, broken windows, tables, and chairs become collateral damage during the altercation - our immune system does the same thing when encountering gluten. No organ is safe during these battles royale. With every ingestion of gluten, our bodies take a pounding. It’s no wonder we feel like crap after eating it. Imagine the amount of damage after years or decades of these conflicts. In some cases, our bodies simply can't recover.
Just as bad environments and neglect cause a building to crumble and collapse, the same will happen to our bodies if we do not strictly follow a gluten-free lifestyle. With knowledge, commitment, and attention to our diet, we can renovate The Crypt into a thriving place like Club 99.

Lack of Support From Family-
http://bit.ly/GIGECW_LackofSupport
Educating Family & Friends About Gluten-Free-
http://bit.ly/GIGECW_EducatingFamilyFriends
“Surprises from Celiac Disease” https://bit.ly/2WFmefu![]()
The Tale of Two Nightclubs PDF
Mood, Behavior, Mental Illness and Gluten

The intent here is not to bore you with medical mumbo jumbo [WARNING: medical mumbo jumbo lies ahead], but the takeaway here is simply this:
Gluten has been shown to affect mood, behavior, and cognitive function.
"The gut is not like Las Vegas. What happens in the gut, does not stay in the gut." ~ Dr. Alessio Fasano
Remember, gluten can affect any, and every organ in the human body – the brain and nervous system are not exempt – even without the presence of celiac disease. Science & medicine are discovering more connections as time goes on.
The statistics for mental illness in the United States are staggering.
- One in four [25%] adults experience mental illness in a given year.
- One in 17 [approx 6%] live with serious conditions like: schizophrenia, major depression, bipolar disorder.
- Approx. 1.1% of adults live with schizophrenia.
- Suicide is the tenth leading cause of death in the US (more common than homicide) and third leading cause for ages 15 to 24 year olds.
- More than 90% of those who die by suicide had one or more mental disorders
- In 2010, the Center for Disease Control reported 38,364 suicides per year – about 14% more than motor vehicle crashes.
- $193.2 billion – Lost earnings per year due to mental illness.
- Veterans account for 20% of suicides. 22 per day.
- Mood disorders (like depression) are the third most common cause of hospitalization for youth and adults 18 to 44.
After looking at those statistics, sadly, I suspect just about every family has had some experience with mental health issues in some form, be it directly or indirectly. I am no exception. My father was a diagnosed Paranoid Schizophrenic. Like many, he was not compliant with his medication regimen nor did he seek on-going professional help. The consequences of his choices are still rippling outward today, almost 50 years after his suicide. I will always wonder if removing gluten would've altered our family's history; without question it has altered my future.
Most mainstream medical professionals do not associate gluten with neurological/behavioral disorders. This is unfortunate because Dr. Marios Hadjivassiliou, Professor of Neurology at Sheffield, UK Teaching Hospitals, stated in 2002,“Gluten sensitivity can be primarily and at times exclusively a neurological disease.” http://bit.ly/1qXJdf3
Dr. Hadjivassiliou has done extensive work with a neurological condition called Gluten Ataxia. This condition is characterized by the loss of balance and coordination, visual disturbances, tremors, difficulty in walking. Living Without Feb/March 2011 has an excellent article on this topic - http://bit.ly/1u24c0q
Dr. Hadjivassiliou is not alone in his discoveries. Dr. Rodney Ford, a Pediatric Gastroenterologist/Allergist from Christchurch New Zealand, wrote this medical hypothesis paper in 2009 titled - “The Gluten Syndrome: A Neurological Disease” - http://bit.ly/1tkM58j
“Gluten can cause neurological harm through a combination of cross reacting antibodies, immune complex disease and direct toxicity. These nervous system affects include: dysregulation of the autonomic nervous system, cerebella ataxia, hypotonia, developmental delay, learning disorders, depression, migraine, and headache. If gluten is the putative harmful agent, then there is no requirement to invoke gut damage and nutritional deficiency to explain the myriad of the symptoms experienced by sufferers of celiac disease and gluten-sensitivity. This is called ‘‘The Gluten Syndrome” ~ Dr. Rodney Ford.
Dr. Ford has devoted an entire book on the subject of gluten's effect on our brains. I highly recommend “Gluten Brains” - http://bit.ly/GlutenBrains
“Neurologic and Psychiatric Manifestations of Celiac Disease and Gluten Sensitivity”was published in Psychiatric Quarterly in March 2012 and contains a great summary of a variety of gluten-related conditions. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641836/
Neurologic Complications include:
- Gluten Ataxia
- Epilepsy and Seizure Disorders
- Peripheral Neuropathy
- Inflammatory Myopathies
- Myelopathies
- Headache
- Gluten Encephalopathy (Brain Damage)
- White matter abnormalities
Psychiatric Complications include:
- Anxiety Disorders
- Depression and Mood Disorders
- Attention Deficit-Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorders
- Schizophrenia
The Celiac Disease Foundation created an excellent resource on celiac disease (and non-celiac wheat/gluten sensitivity) and mental health. It's meant to be shared with healthcare providers.
http://ow.ly/en1M30ghVy8
A wide range of psychological problems can arise for those with untreated celiac disease or non-celiac wheat sensitivity. Initially there may be a misdiagnosis of psychiatric illness due to some of the neurological and psychiatric symptoms that can be seen in untreated disease. Once diagnosed, there may be difficulty adjusting to a new diagnosis of chronic illness and adherence to a gluten-free diet."When a Mental Health Referral Is NeededA wide range of psychological problems can arise for patients with untreated celiac disease or non-celiac wheat sensitivity. These can include difficulties adjusting to a new diagnosis of chronic illness as well as dealing with adherence to a gluten-free diet and other aspects of disease management. Protracted duration of emotional or behavioral symptoms, greater severity of symptoms, and/or significant impairment in functioning are indicators of potential need for mental health treatment. These include:
• Finding little or no pleasure in life • Feeling worthless or extremely guilty • Crying a lot for no particular reason • Withdrawing from other people • Experiencing severe anxiety, panic or fear • Having big mood swings • Experiencing a change in eating or sleeping patterns • Having very low energy • Losing interest in hobbies or pleasurable activities • Having too much energy, having trouble concentrating or following through on plans • Feeling easily irritated or angry • Experiencing racing thoughts or agitation • Hearing voices or seeing images that other people do not experience • Believing that others are plotting against you • Wanting to harm yourself or someone elseWhen A Medical Evaluation Is NeededInitially those with celiac disease or non-celiac wheat sensitivity may be misdiagnosed with a psychiatric illness due to some of the neurological and psychiatric symptoms that can be seen in untreated disease including:• Mood changes • Anxiety • Fatigue • Difficulties with concentration and attention • Sleep difficulties • Decrease appetiteCeliac Disease and Gluten-Related Conditions Psychological Health Training ProgramThe Celiac Disease and Gluten-Related Conditions Psychological Health Training Program was created by the Children’s National Health System in partnership with Celiac Disease Foundation, and was made possible by a generous grant from the Resnick Family. This continuing education program provides a tool kit for medical and mental health practitioners to identify and treat patients living with celiac disease and other gluten-related conditions.Watch the Psychological Health Training Program Webinarhttp://bit.ly/2hI3QgTPsychological Health ManualAvailable both as an interactive manual and as a pdf document, the goal of this manual is to increase medical and mental health providers’ awareness of celiac disease and non-celiac wheat sensitivity in pediatric populations. However, it’s lessons apply to adult populations, and is a useful tool for patients and caregivers to better understand the disease.Read the Psychological Health Training Program Manualhttp://bit.ly/2iwf2wV
Depression
Depression is a medical condition that interferes with daily life; affecting thoughts, feelings, behavior, mood and physical health for extended periods of time. Some people may only have one episode of major depression in their lifetime, but often times it is a recurrent issue.
In celiac disease, nutritional deficiencies from intestinal damage may also contribute to depression. Lack of B-vitamins, specifically B-12 and folic acid have been linked.
Reports of depression in those with celiac disease began appearing in the 1980s. In 1982, a Swedish study reported “Our results suggest that depressive psychopathology is a feature of adult coeliac disease and may be a consequence of malabsorption” http://1.usa.gov/W3jKEB
A 1998 study shows about one third of diagnosed celiac patients also suffer from depression. Celiac adolescents have higher than normal rates of depression (31% vs 7% of adolescents without celiac). http://bit.ly/1qUGi2S
A large Swedish study published in 2007 compared almost 14,000 celiac patients against almost 67,000 healthy people. Researchers found that celiacs are 80% more likely to experience depression than the general population. They also looked at the celiac-depression relationship in reverse. They found those with depression had a 230% increased risk factor of having celiac disease. http://1.usa.gov/1pApGlN
Women with celiac disease have higher rates of depression than the general population. The risks were highest in those that were not compliant with the gluten-free diet. Even when compliant, women still had higher risks of depression over those without celiac. http://bit.ly/W3nKoE
According to Dr. Tom O'Bryan, children have a 40% increase risk of suicide. Those children with intestinal inflammation [no villi damage yet] have a 96% increased risk. http://bit.ly/1rJ7wjo
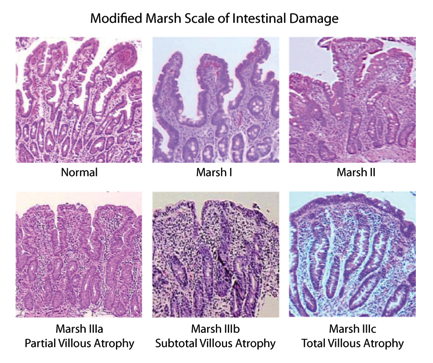
Adults diagnosed with celiac disease and/or intestinal inflammation have increased suicide risks as well. Another large study published in 2011 from Sweden shows those with with celiac disease [intestinal damage] had a 55% increased risk factor. Those with intestinal inflammation [no villi damage] had a 96% increased risk. http://1.usa.gov/Z4DFFk
More Gluten & Depression Studies
“A study has now demonstrated that gluten is independently associated with depression in patients with NCGS.” - http://1.usa.gov/1tZiAqc
“Exposure to gluten specifically induced current feelings of depression.” - http://1.usa.gov/1ucfDBZ
“Lifetime depressive symptoms may be present in one third of the CD patients who adhere to gluten-free diet. Long-term adherence to the gluten-free diet may reduce the risk of current depressive symptoms.” - http://1.usa.gov/1qqWZpe
Schizophrenia
Schizophrenia is a brain disorder that distorts thinking, behavior, emotions, the perception of reality. Delusions [believe people are try to control them or plotting against them] and hallucinations [hearing voices] are common symptoms.
There have been observations of Schizophrenia and gluten dating back to the 50's & 60's – also known then as “Bread Madness”.
In 1953 Dr Lauretta Bender started seeing increased incidences of celiac disease in those with childhood schizophrenia.
In 1961 Harold Graff, M.D. and Allen Handford M.D. published the case study, “Celiac Syndrome in the Case Histories of Five Schizophrenics”, about five patients with a history of schizophrenia and celiac disease who happened to be admitted to the same psychicatric hospital over the course of 365 days. A most curious observation in facility that had few admissions over the course of a typical year. http://bit.ly/1uFm56w
Dr. F. Curtis Dohan spent most of his career drawing connections between wheat and schizophrenia. He too noticed a number of patients with schizophrenia also had celiac disease – potentially 50 to 100 times the rate that would be expected by mere chance. Beyond these connections, he reported that a gluten-free diet improved some of the newly diagnosed schizophrenics, but not all. 2 out of 17 improved. http://bit.ly/1nhCHLw
In 1966 Dohan published “Wheat Consumption and Hospital Admissions for Schizophrenia During World War II”. He analyzed the the decreases in hospital admissions for schizophrenia during the wheat shortages in Finland, Norway, Sweden, Canada and the United States during World War II. http://bit.ly/1q0nRxU
Like many pioneers in their field, Dohan was often ridiculed and marginalized for his work [opioid research in mental illness], but he continued publishing his findings. Dohan also demonstrated that schizophrenia was almost non-existent in South Pacific cultures where little to no grains were consumed. When those cultures began to westernize their diet with the consumption of wheat, barley beer, and rice, the prevalence reached European levels. http://1.usa.gov/1wYpKja
Did Dohan find a “scientific smoking gun” linking gluten and schizophrenia – not exactly according to some experts, but his work is now proving to be quite interesting and now beginning to be validated.
It has only been over the last decade or so that experts have shown gluten's effects on the nervous system. Even to this day experts are still looking indisputable evidence connecting the two conditions.
In 2012, another study revealed that people with schizophrenia are much more likely than the general population to have an immune response to gluten. When those with schizophrenia and a documented immune response to gluten tried a gluten-free diet, they got better. These results are very promising for those suffering from a neuro-degenerative condition where little else works.
Not everyone with schizophrenia will see improvements on a gluten-free diet. New research is indicating about 20% may experience measurable improvements. Dr. Alessio Fasano's team have found that roughly 1 in 5 patients with schizophrenia have elevated levels of tTG6 (a new marker indicating gluten-sensitivity). Those patients put on a gluten-free diet were able to control their condition without medication. Promising results indeed!
More Gluten & Schizophrenia Studies
“Gluten Sensitivity and Schizophrenia” a PowerPoint presentation by Deanna Kelly, Pharm.D, BCPP Professor of Psychiatry at Univ. of Maryland School of Medicine.
http://bit.ly/2f4x8pv
“Emerging scientific literature contains several reports linking gluten sensitivity states with neuropsychiatric manifestations including autism, schizophrenia, and ataxia.” http://1.usa.gov/1tkxTvQ
“A drastic reduction, if not full remission, of schizophrenic symptoms after initiation of gluten withdrawal has been noted in a variety of studies. However, this occurs only in a subset of schizophrenic patients.” - http://bit.ly/2kIpUtQ
“Five biomarkers of gluten sensitivity were found to be significantly elevated in patients with non-affective psychoses (schizophrenia) compared to controls.” - http://1.usa.gov/1vXlWL1
Al Klapperich
Branch Manager
Gluten Intolerance Group of East Central WI
Updated: 11/05/17 - Add Celiac Disease Foundation information.
Updated: 02/12/17 - Fix broken schizophrenia study linkUpdated: 11/05/16 - Updated Deanna Kelly's presentation link.
Updated: 10/09/16 - Add Susan William's letter.